Why is Credentialing Important?
Medical credentialing is significant in light of the fact, as the process offers patients a chance to certainly confide in their selected physicians. It means providers are vetted for their education, degrees, work history, behavior, and other legalities before they become part of a payer network. Similarly, before a provider joins an organization, hospital or a surgery center, their documents and degrees are verified by a credentialing substance.
Frequently discussed alongside with medical credentialing is the process of enrollment. It is the process of applying to the insurance network to be included in their panel of providers.
Preciso Credentialing benefits
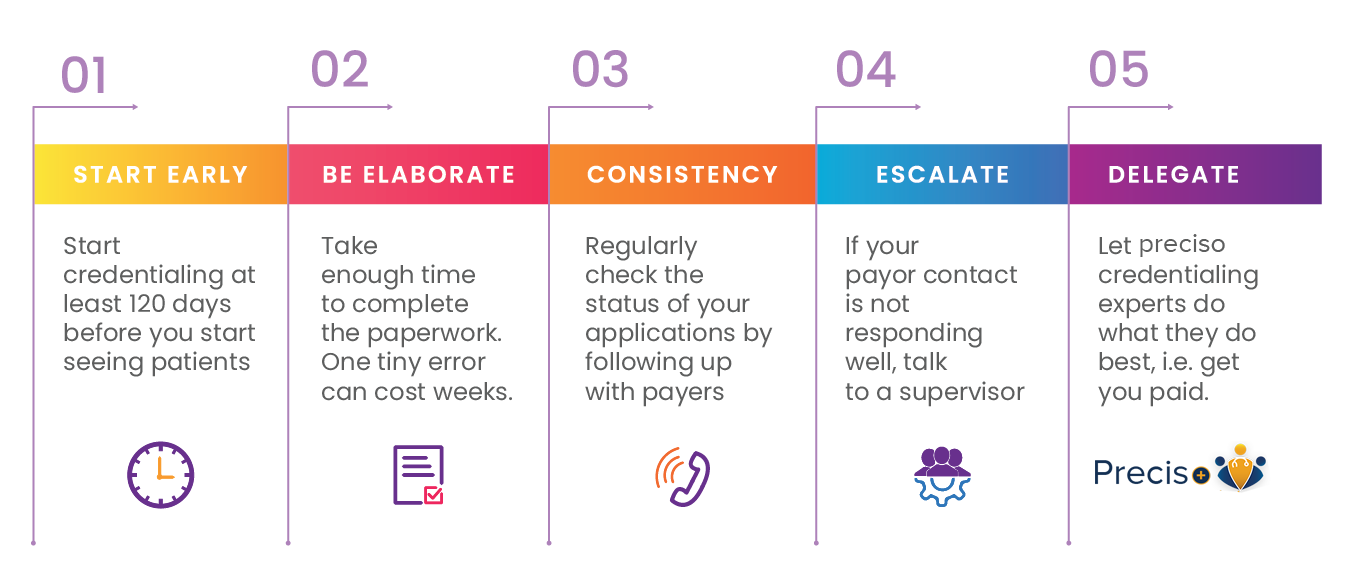
Steps in Provider Credentialing
- Saves you months of time and work.
- Eliminates the aches and pains caused by vast amounts of printed materials and applications.
- Increases patient referrals.
- Speeds up payments by the insurance companies.
- Assigns a dedicated project manager to your venture
- Makes telephone calls, subsequent follow-ups presents all applications, messages, and emails.
- All-time access to online project portals.
- Provide you with a cost-competitive edge to help your practice grow.
How process will work?
Free yourself from all the worries, piles of printed material, and perplexity with the insurance agencies. Preciso Healthcare Solutions are credentialing specialists going above and beyond to explore the troublesome procedure of a provider credentialing. Preciso gives providers credentialing administration at an unparalleled cost. Our service also incorporates primary source check. We work with on behalf of physicians and specialties at the same time.
Whether you want to get credentialed for insurance systems like Medicare, Medicaid, or commercial insurance payors, we can get you vetted as early as possible so that you start getting paid. Our arrangement fits any association paying little heed to their size or specialty. If you are an individual or a medical group, Preciso medical credentialing services would keep you updated efficiently.
The Center for Affordable Quality Healthcare, INC. (CAQH)
CAQH is the go-to organization when it comes to provider’s records verification. It is one of the most-used online services for credentialing.
If you have any questions regarding the process, please visit the organizational link here: http://www.caqh.org/updFAQ.php
However, in case you don’t have a third-party intermediary to look after and you are credentialing on your own, it’s best to maintain a provider credentialing checklist to ensure the process happens as smoothly as possible.
